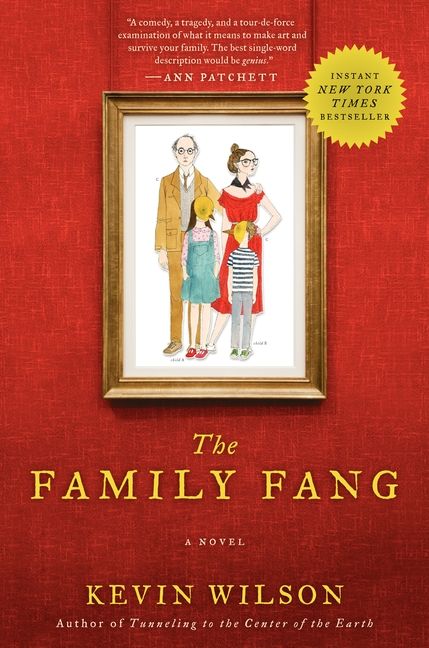
Family Fang (2016) Online English
- 17 Comments!

The Family Fang (2. IMDb. Edit. Annie and Baxter, the adult children of the controversial husband and wife conceptual performance art couple famous for their quirky macabre public performances, have never got over the fact that their parents kept using them during their childhood in their often gory and disturbing satirical public performances. They often clash with their now elderly parents over this and blame them for their problems in their adult life.
However, the two become worried when they're told by the police that their parents have gone missing during their trip outside of town. The brother considers the possibility that something horrible might have happened to them, but the sister is convinced that it's just another one of their stupid games or twisted conceptual performances. She convinces him that they should go and look for them themselves.
Genetic Atypical Hemolytic- Uremic Syndrome - Gene. Reviews. Typical HUS is triggered by infective agents such as certain strains of E. However, approximately 2.
Hypophosphatasia is characterized by defective mineralization of bone and/or teeth in the presence of low activity of serum and bone alkaline phosphatase.
Yao Chen was born in Shishi City, Quanzhou, Fujian province, China on October 5, 1979 to a middle-class family, and studied Chinese folk dance at the.
Crimson Fang is an uprising located in Port Nowhere and filled with smugglers and mercenaries. Jor “Oneshot” Mesok. HP:966k (Story) Jor immediately teleports on. Singapore Indoor Stadium
HUS is diarrhea negative. During an acute episode, identification of Shiga toxins in the stools (by the Vero cell assay) and/or serum antibodies against Shiga toxin (by enzyme- linked immunosorbent assay . The detection of free fecal STEC (Shiga toxin- producing E. Approximately 8. 0%- 9.
Survival China Travel Tips and Tricks. These China Travel Tips, Survival Techniques, will help you get around and make your trip to China easier, so you will be able. First translated during the summer of 1990. Revised 2017-05-09. When citing, please refer to the URL of this page: http://www.acmuller.net/con-dao/analects.html.
HUS) or after plasma infusion or exchange (as in adult or severe forms of typical HUS) . Typical HUS usually subsides when the underlying condition is treated or removed. Note: STEC isolation and detection of LPS antibodies are not routinely available and require a few days to complete.
Distinguishing a. HUS from thrombotic thrombocytopenic purpura (TTP). Atypical HUS and TTP (OMIM 2. In a. HUS the lesions and clinical symptoms are mainly localized in the kidney, whereas the pathologic changes of TTP are more extensively distributed. Clinically, TTP manifests mainly with central nervous system symptoms, but renal insufficiency has been reported.
Approximately 8. 0% of TTP is triggered by deficient activity of ADAMTS1. ADAMTS1. 3 deficiency can be constitutive, as a result of biallelic. ADAMTS1. 3 pathogenic variants; or acquired, as a result of an inhibitory antibody. Evaluation of ADAMTS1. VWF multimers in vitro (e.
Deficiency of ADAMTS1. HUS . The exception occurs when ADAMTS1. CFH pathogenic variants are observed in the same individual.
Affected individuals with both ADAMTS1. CFH pathogenic variants have been reported . C3. G is identified by glomerular changes in which there is C3 dominant staining at immunofluorescence, with absence or near absence of immunoglobulins. The two major subgroups of C3. G include dense deposit disease (DDD) and C3 glomerulonephritis (C3. GN). Clinically, C3. G presents with proteinuria, hematuria, and often some degree of renal failure.
In DDD, acquired partial lipodystrophy and ocular drusen may also be seen. Median age at C3.
G diagnosis is 2. DDD presents earlier with a mean age at diagnosis of 1. Ten- year progression to ESRD is higher in DDD (3.
C3. GN (2. 5%). Recurrence of disease and allograft loss after transplantation is common (5. C3. Nefs are found in 6. C3. G . Also anti- CFH autoantibodies have been identified in a few individuals with C3.
G. Multiple genetic causes have been reported in individuals with C3. G. These include biallelic. CFH pathogenic variants that cause severely reduced CFH protein levels found in autosomal recessive cases of DDD or C3. GN . Furthermore, this overlap in phenotypes is evident in those few individuals who have a mixed diagnosis of a. HUS and C3. G in the same biopsy or in biopsies taken at different points in time . Cobalamin C disease is associated with pathogenic variants in MMACHC. It is characterized by abnormal vitamin B1.
HUS . Inheritance is autosomal recessive. See Disorders of Intracellular Cobalamin Metabolism. Management. Current guidelines for the initial assessment and early management of children with a. HUS have been published . Eculizumab should be considered as a first- line therapy when the diagnosis of a. HUS is unequivocal, since this treatment has the potential to rescue renal function when administered early after onset of the disease .
Cohort data show that response to plasma therapy was in part related to the genetic background of the treated patient . Despite the variability in response to therapy, plasma therapy is the only therapy with near- complete global availability and therefore it remains an important treatment for a.
HUS. Plasma therapy should be started as soon as a. HUS is suspected and continued until resolution of thrombotic microangiopathy. In individuals who respond, plasma exchange can be gradually withdrawn, although a significant proportion will require continued plasma exchange to maintain remission.
There is minimal evidence to suggest the superiority of either plasma exchange or plasma infusion, and instead the selected option should be based on individual tolerance, local expertise, and resources (e. Typically, plasma exchange is undertaken daily initially; the duration and frequency of treatment is then determined by the clinical response. Treatment can be intensified by increasing the volume of plasma replaced. Twice- daily exchange of one plasma volume is probably the treatment of choice for those with refractory disease in order to minimize the recycling of infused plasma. Plasma infusion is the first- line therapy when plasma exchange or eculizumab therapies are not available. In plasma infusion 3.
L/kg of plasma is administered initially, followed by 1. L/kg/day. Plasma infusion should be used to treat or prevent recurrent episodes. Platelet count and serum LDH concentration are the most sensitive markers for monitoring response to plasma therapy. Plasma treatment should be continued until platelet count and serum LDH concentration remain normal after therapy is discontinued. Discontinuation of plasma therapy is the only way to know if complete remission has been achieved.
Immediate exacerbation of disease activity, principally manifested by falling platelet count that requires the resumption of daily plasma therapy, occurs in 2. Thus, many cycles of stopping and resuming plasma therapy may occur, in which case therapy with eculizumab should be considered. Genetic characterization of persons with a. Garbage Pail Kids Story (2017) Online English. HUS has the potential to optimize the treatment: C3.
Response to plasma treatment in persons with C3 pathogenic variants was comparable (5. CFH pathogenic variants . It is hypothesized that plasma exchange could remove mutated hyperactive C3 and also provide regulatory plasma proteins to counteract complement activation induced by mutated C3. CD4. 6. The rationale for using plasma in individuals with CD4.
CD4. 6 protein (also known as MCP) is a transmembrane protein and, theoretically, plasma infusion or plasma exchange would not compensate for the MCP defect. Published data indicate that the majority (8.
The decision whether or not to treat with plasma should be based on the clinical severity of the acute episode. CFH. Plasma infusion or exchange has been used in individuals with a. HUS and CFH pathogenic variants with the rationale of providing normal CFH to compensate for the genetic deficiency, as CFH is a circulating plasma protein. In published studies, some individuals with CFH pathogenic variants did not respond at all to plasma therapy and died or developed ESRD. Others required infusion of plasma at weekly intervals in order to raise CFH plasma levels enough to maintain remission . One year after discontinuation of plasma therapy, the patient remained disease free and dialysis independent.
A dozen case reports showed that early plasma therapy, generally consisting of daily plasma exchange followed by maintenance plasma exchange/infusion, could prevent relapses and preserve renal function at follow up for up to six years . However, the remaining individuals did not respond at all to plasma and 2. In the French cohort . In individuals with anti- CFH autoantibodies, plasma treatment induced complete or partial remission (normalization of hematologic parameters with renal sequelae) of 7.
Persons with anti- CFH autoantibodies benefit from treatment with steroids or other immunosuppressants in conjunction with plasma exchange. CFI. Theoretically one should expect a good response to plasma therapy in individuals with CFI pathogenic variants because CFI (like CFH) is a circulating protein; the results, however, suggest that a larger quantity of plasma is required to provide sufficient wild- type CFH or CFI to compensate for the genetic deficiency . Indeed, remission was achieved in only 2. CFI pathogenic variants . Absence of evidence linking DGKE deficiency to the complement cascade and relapses of acute a.